Diagnostics for Antimicrobial Resistance in Low- and Middle-Income Countries
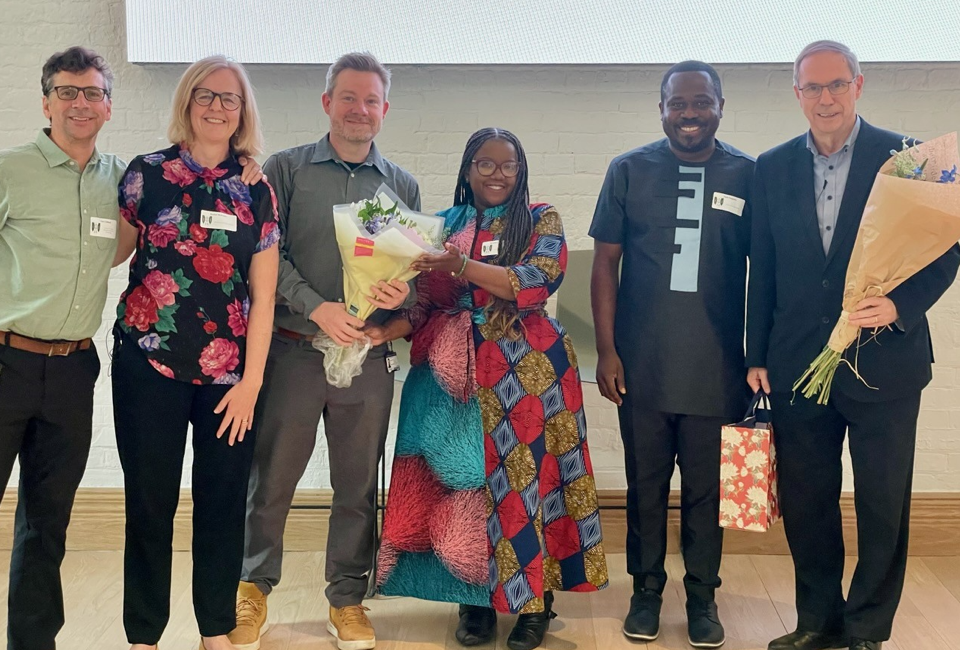
In July, the excellent Diagnostics for Low- and Middle-Income Countries (LMICs) international Conference was hosted by Professor Lord Tarassenko in Reuben College Oxford University, and co-chaired by Professor Rachel McKendry (UCL) and Professor Gari Clifford (Emory University & Georgia Institute of Technology). UCL Provost and President Professor Michael Spence sent a video message with his support for the conference.
The two-day conference focused on catalysing the development and delivery of new diagnostics for LMICs and brought together over 100 researchers from around the world. Day 1 focused on Diagnostics for Antimicrobial Resistance (AMR) including a joint session with Oxford International Pandemic Sciences Institute Conference and after dinner talk by Professor Kevin Marsh and Dr Anne Makena (AfOx initiative). Day 2 was chaired by Professor Clifford and Professor Philip Fowler (Oxford University) and welcomed speakers focusing on Diagnostics for Tuberculosis, Sepsis as well as Data Science and AI for diagnostics, including Dr Gordon Sanghera (CEO of Oxford Nanopore) and many more.
The opening session on Diagnostics for AMR in Africa was chaired by Professor Rachel McKendry and Dr Noah Fongwen (Africa CDC), with funding from the EPSRC Digital Health Hub for AMR. AMR is a global problem, but new research suggests that Africa has the highest burden of AMR in the world with an estimated 1 million deaths each year. Yet historically the scale of the AMR challenge in Africa has been underestimated and underfunded.
Talks from Dr Noah Fongwen (Africa Centres for Disease Control and Prevention & London School of Hygiene and Tropical Medicine) highlighted the key role of Africa CDC and their strategy to accelerate diagnostic access for priority diseases of epidemic potential that will be applicable to AMR tests in future, including a network of evaluation sites and regulatory harmonization to allow for procurement and stockpiling of diagnostics. Locally manufactured tests will be prioritised. Dr Brenda Kwambana (Malawi Liverpool Wellcome Programme and UCL) spoke about her exciting new NIHR programme on AMR which aims to advance diagnostics solutions for respiratory pathogens and AMR in Sub-Saharan Africa. Her talk highlighted three diagnostics bottle necks including i) sample collection, transportation and storage, ii) diagnostic testing and interpretation, and iii) data reporting and sharing, as well as the unaffordability and lack of infrastructure meaning that many technologies are frequently not well-adapted to resource-limited settings and require further validation. Professor Maryam Shahmanesh from UCL and the Africa Health Research Institute gave a talk on diagnostics for AMR emphasising the importance of co-development and rigorous evaluation lessons from HIV. During the joint session, Professor Rachel McKendry gave an overview of the Digital Health Hub for AMR and highlighted the need for connected tests for AMR, citing the 100 Days Mission for Diagnostics. She spoke about her research harnessing machine learning to capture and classify results from lateral flow tests, working in partnership with the Africa Health Research Institute on HIV rapid tests, and the REACT study on COVID rapid tests.
During the open panel discussion, the need to engineer better diagnostics tests and decision support tools for antimicrobial stewardship and AMR surveillance was discussed as well as the challenges facing Africa including limited diagnostics and digital infrastructure, as well as institutional and workforce skills and capacity. The discussions highlighted the diagnostics data gaps, the challenge of over-the-counter antibiotic sales and the need for significant AMR educational and awareness campaigns. The rise of AMR – also known as the silent pandemic – knows no geographical boundaries and the lessons learned from the COVID-19, are that no one is safe until we are all safe.
Day 2 began with an excellent introduction from Hamish Fraser (Brown University) covering the use of AI to predict loss to follow up of HIV patients in Kenya by the AMPATH clinical research and informatics teams. Professor Michelle Heys provided a deep dive into her team’s amazing work with researchers in Zimbabwe on Neotree for neonatal sepsis diagnosis in sub-Saharan Africa. Dr Gordon Sanghera provided an exciting update (and show-and-tell) on Oxford Nanopore’s efforts to enhance widespread access to DNA and RNA sequencing. Professor Gari Clifford kicked off the afternoon with and introduction to data science and AI for diagnostics in LMICs, illustrating this with his collaborations on safe+natal, for improving birth outcomes with indigenous midwives in rural Guatemala. Professor Ester Sabino (University of São Paulo Medical School) then provided an insight into a remarkable telemedicine system developed with colleagues in Brazil for screening of Chagas disease through AI-assisted low-cost electrocardiograms. The conference then ended with a panel discussion Dr Anne Makena and Professor Kevin Marsh, drawing on the global south researchers present to help design next year’s event!
We are very thankful to Professor Lord Tarassenko and Reuben College Oxford University for providing generous funding for this exceptional conference, which enabled UCL students from LMICs including South Africa, Gambia, Malawi, Nigeria, Morocco, India, Indonesia, Argentina, Russia, Iran, Chile and Malaysia to participate. More information about the event be found here: https://reuben.ox.ac.uk/event/diagnostics-lmics-conference-2024